The Viral Research and Diagnostic Laboratory Network of the Department of Health Research, coordinated by the Indian Council of Medical Research and NIV, and the Integrated Disease Surveillance Programme led by the National Centre for Disease Control, have emerged as key players in the surveillance of viral and other diseases in India
Viruses claimed new territory in India in 2018. As usual, they treated man-made geographical boundaries with sheer disdain. Two viruses which were in the spotlight and led to outbreaks this year were the Nipah and Zika. Both outbreaks were detected in a timely manner and controlled through the coordinated and remarkably successful efforts of various agencies of the State and Centre.
In addition to general physicians and specialists (neurology, pulmonary medicine, obstetrics, community medicine, microbiology and virology) from the public and private sectors, as well as nurses, those who contributed to these efforts included veterinary doctors and scientists, epidemiologists, entomologists, administrators, security personnel and the media. The scale of operations is evident from the wide range of skillsets used to stop these outbreaks from spreading further.
The outbreak of Nipah infection was localised to Kozhikode and Malappuram districts of Kerala. The patients presented with the symptoms of encephalitis and respiratory distress. Nineteen cases of Nipah occurred in the State between mid-May and early June. Due to the inherently high mortality associated with this infection, 17 patients succumbed to the illness, including Lini Puthussery, a nurse who had diligently attended to affected patients, once again highlighting the risks faced by healthcare personnel in their fight against infectious diseases.
The National Institute of Virology, Pune, rapidly confirmed the diagnosis by amplifying and detecting the ribonucleic acid (RNA) of the Nipah virus using a now widely-used technique called real-time polymerase chain reaction. They could also detect immunoglobulin M (IgM) antibodies specific to the virus, which appear early in the disease, by an enzyme-linked immunosorbent assay. All contacts of the patients were followed closely and, if infected, were isolated, tested and given supportive treatment. Unfortunately, as of now, there is no commercially available vaccine or specific anti-viral drug against Nipah.
Pteropus species fruit-eating bats, which are a known reservoir of the Nipah, were also collected from areas near the index case’s house in Kozhikode, Kerala. Ten of these 52 bats tested positive for the virus. Nipah can be acquired by consuming partially-eaten fruits, date palm sap or fresh palm toddy contaminated with the saliva (or urine) of infected bats, by direct contact with infected bats or their faeces or urine, and by close contact with infected patients at home.
Fruit bats were also implicated in transmission during the two previous outbreaks of Nipah in West Bengal in 2001 and 2007, as well as infrequent outbreaks in Bangladesh in the past. These bats are distributed across most of the Indian subcontinent and South-East Asia, carrying a potential threat of spreading the Nipah, if infected. However, in the first outbreaks in 1998-1999 in Malaysia and Singapore, pigs rather than bats were implicated in the transmission cycle.
In both geographical locations, this viral infection emerged as an important viral zoonotic disease. These are diseases which can infect and be transmitted between animals and humans. Since a large number of infectious diseases, including other viral diseases like influenza and rabies, are zoonotic, the World Health Organisation has rightly been promoting a — One Health — approach, in which all stakeholders from animal and human health, as well as food safety, work together to combat these infections.
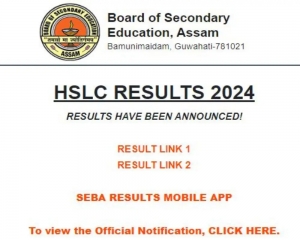
India was declared Nipah free at the end of July and within less than two months the next viral outbreak hit the country. This time it started with a confirmed case of Zika in Jaipur. Previously, in May 2017, three cases of Zika infection were found during surveillance in Gujarat, and one in Tamil Nadu. Since the reports of the Zika epidemic in Brazil, testing for Zika was being carried out as a part of surveillance in fever cases of a short duration across India. However, no other Zika cases were found in the interim period, despite large scale screening of samples.
The Zika causes either asymptomatic infection or just a fever similar to dengue, which does not carry the risk of worrisome, though rare and immediate complications like bleeding and shock. Deaths have not been known to occur due to this infection. One would not have been unduly concerned about this infection, had the 2015 epidemic in Brazil (which was due to a variant of the Asian lineage of the virus) not been associated with a risk of birth defects.
These included microcephaly (a small-sized head, with the risk of a poorly developed brain) in babies born to women infected during pregnancy. The virus was known to circulate in Asia and Africa since the 1960s, but no outbreaks or complications were reported earlier. Rare neurological complications were also seen in the Brazilian epidemic in adults and older children for the first time.
For the diagnosis of suspected cases of Zika, the viral RNA is detectable in the blood by real-time PCR only during the first week of illness or so, after which anti-Zika antibodies appear and the virus is mopped up, becoming undetectable. However, reliable antibody detection tests are not commercially available for the detection of Zika antibodies at a later stage of the infection.
In Jaipur, the diagnosis of Zika was first made at the virology laboratory of the SMS Medical College and then confirmed by NIV, Pune. Numbers escalated quickly after the index case and spiraled up to more than 150 cases. Interventions against mosquito breeding had to be implemented on a war footing, along with active surveillance and testing of all pregnant women, as well as fever cases and their contacts for Zika. Through these measures, it was possible to keep the infection more or less confined to a single specific locality in Jaipur, and to eventually control the outbreak. No cases of microcephaly or congenital Zika syndrome have been reported until now.
The NIV has reported by sequencing the genome of the Indian virus that, though it belongs to the Asian lineage (as in Brazil), it does not carry some of the signature sequences which were associated with microcephaly. However, the risk can’t be completely ruled out yet and the infected pregnant women in Jaipur will need to be closely monitored through their pregnancy and their babies examined and tested.
Zika infection is spread by a familiar enemy, the female Aedes mosquito, which can also transmit Dengue and Chikungunya when it bites humans for its blood meal, depending on which virus it may be infected with. The breeding (and transmission) season is during the monsoon in North India, but may persist throughout the year in South India. The habits of this mosquito are familiar to most. It usually bites during the day, particularly at dusk and dawn (but that does not mean it cannot bite at night). It breeds in relatively clean water and a collection of a teaspoon or two of water is enough to allow eggs to be laid and larvae to grow.
It is a primarily urban mosquito with a flying range of only a couple of hundred metres. This means it remains close to where it hatches and breeds, to spread infection in the vicinity of the breeding site. This breeding can only be controlled by the active involvement of the community, if we look for and remove all breeding sites in and around our homes and workplaces. As individuals, we can protect ourselves with mosquito repellents and by covering ourselves, day and night.
The timely detection of these two viral outbreaks in 2018, with the quick diagnosis of their cause, and the rapid, successful deployment of control measures, utilising a wide range of resources, has been most heartening. It highlights the rapidly maturing and efficient disease surveillance networks, which have been created in the country over the last decade, along with a well-oiled infectious outbreak control machinery,.
The Viral Research and Diagnostic Laboratory Network of the Department of Health Research, coordinated by the Indian Council of Medical Research and NIV, and the Integrated Disease Surveillance Programme led by the National Centre for Disease Control, have emerged as key players in the surveillance of viral and other diseases in India. Viruses are here to stay and will keep challenging us with potential and real threats, but India is doing its best by remaining in a continuous state of preparedness. This battle is always on.