Instilling hope in millions of people with the sickle cell disease (SCD) across the world including India, which has the second-highest prevalence of the blood genetic abnormality, Britain's medicines regulator has recently authorized the world’s first gene therapy treatment for the Sickle cell and a type of sickle cell disease called beta-thalassemia in the UK. THE HEALTH PIONEER reports
SCD is marked by chronic anaemia, recurrent episodes of intense pain requiring hospitalisation, organ damage, an elevated risk of stroke, and premature mortality. As of 2021, almost 8 million people around the world live with SCD.
In India, according to estimates, the tribal population living in southern, central, and western states is particularly susceptible to it. The most endemic states are- Gujarat, Maharashtra, Rajasthan, Madhya Pradesh, Jharkhand, Chhattisgarh, West Bengal, Odisha, Tamil Nadu, Telangana, Andhra Pradesh, Karnataka, Assam, Uttar Pradesh, Kerala, Bihar, and Uttarakhand.
Considering 10 per cent of India’s population lives in tribal areas, it is important to focus on Sickle Cell Anaemia (SCA) detection in this community, say the experts in the sector.
Talking about the recent development in the sector, they inform that the Medicines and Healthcare Regulatory Agency in the UK has approved Casgevy, the first medicine licensed using the gene editing tool CRISPR, which won its makers a Nobel prize in 2020.
The agency approved the treatment for patients with sickle cell disease and thalassemia who are 12 years old and over. Casgevy is made by Vertex Pharmaceuticals (Europe) Ltd. and CRISPR Therapeutics. To date, bone marrow transplants, extremely arduous procedures that come with very unpleasant side effects, have been the only long-lasting treatment. There are very few drugs available for the treatment of sickle cell disorder.
“The future of life-changing cures resides in CRISPR based (gene-editing) technology,” said Dr. Helen O’Neill of University College London.
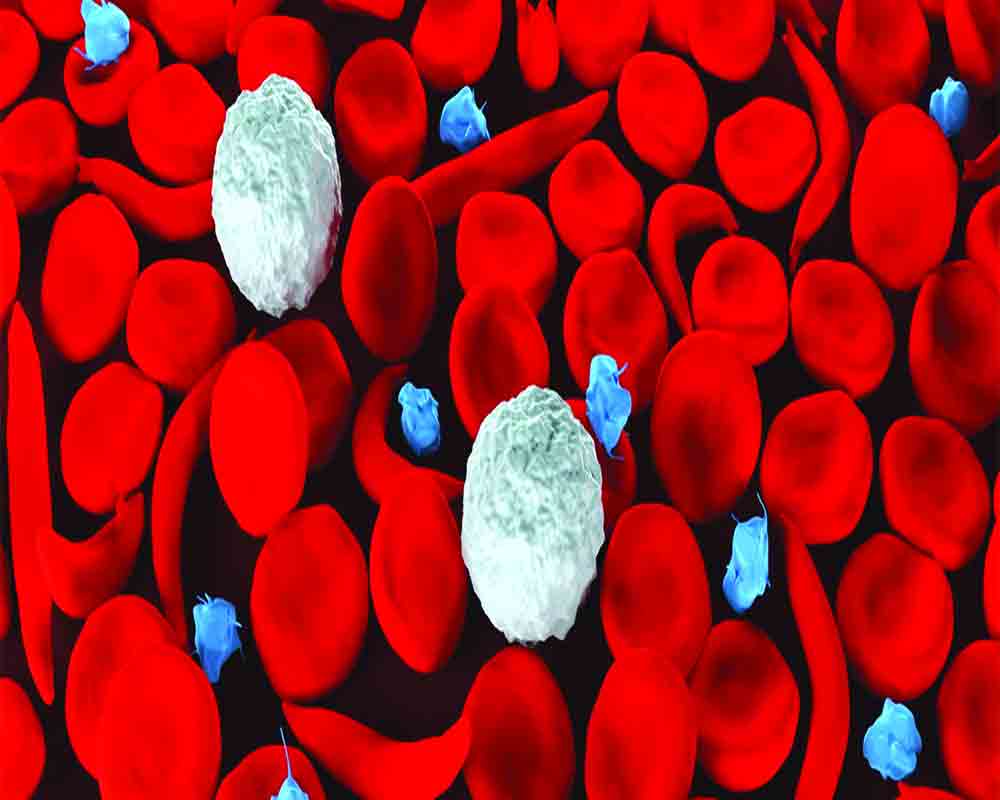
Both sickle cell disease and thalassemia are caused by mistakes in the genes that carry hemoglobin, the protein in red blood cells that carry oxygen.
In people with sickle cell — which is particularly common in people with African or Caribbean backgrounds — a genetic mutation causes the cells to become crescent-shaped, which can block blood flow and cause excruciating pain, organ damage, stroke and other problems.
In people with thalassemia, the genetic mutation can cause severe anemia. Patients typically require blood transfusions every few weeks, and injections and medicines for their entire life. Thalassemia predominantly affects people of South Asian, Southeast Asian and Middle Eastern heritage.
The new medicine, Casgevy, works by targeting the problematic gene in a patient’s bone marrow stem cells so that the body can make properly functioning hemoglobin.
Patients first receive a course of chemotherapy, before doctors take stem cells from the patient’s bone marrow and use genetic editing techniques in a laboratory to fix the gene. The cells are then infused back into the patient for a permanent treatment. Patients must be hospitalized at least twice — once for the collection of the stem cells and then to receive the altered cells.
Britain’s regulator said its decision to authorize gene therapy for sickle cell disease was based on a study done on 29 patients, of whom 28 reported having no severe pain problems for at least one year after being treated. In the study for thalassemia, 39 out of 42 patients who got the therapy did not need a red blood cell transfusion for at least a year afterwards.
Gene therapy treatments can cost millions of dollars and experts have been raising concerns that they could remain out of reach for the people who would benefit most.
In India too, for many, the therapy, for now, may remain unaffordable until government intervention.
Moreover, according to the health experts, its application, using stem cell transplant, is limited to individuals who meet specific criteria. “Consequently, it won’t be a viable option for everyone,” said Sickle Cell Society in a statement.
Last year, Britain approved a gene therapy for a fatal genetic disorder that had a list price of £2.8 million ($3.5 million). England’s National Health Service negotiated a significant confidential discount to make it available to eligible patients.
In many countries like India, current treatment options - hydroxyurea, crizanlizumab, and voxelotor – aim to reduce the frequency of painful crises but they do not alleviate the pain, thus needing strong painkillers. For example, hydroxyurea supports hemoglobin production and has been shown to reduce about half of the number of painful events a person with SCD may experience, as per the experts.
A recent study estimated the life expectancy of adults with SCD to be 54 years, approximately 20 years shorter than that of adults without SCD.
Currently, treatments for SCDS include medications mainly used for pain management and surgical procedures including blood transfusions and bone marrow — also known as stem cell — transplants.
The Government in India on its part has taken various initiatives with an aim to address the blood disorder associated with the shape of red blood cell, rolling out the SCD elimination Mission being the major one. During the Union budget 2023, Union Finance Minister Sitharaman announced the mission to eliminate sickle-cell anaemia by 2047. The project focuses on raising awareness, universal screening of about seven crore individuals—aged 0-40—in afflicted tribal areas, and counselling through combined efforts of central ministries and state governments.
In the meanwhile, the nod to the new gene therapy offers newfound hope and optimism for the sickle cell community, and a step forwards in the fight for an end to inequalities in the treatment of people living with the condition, added the statement from the Sickle Cell Society.
HOW THE NEW THERAPY WORKS
Casgevy is a gene editing therapy. Gene-editing technologies have the ability to make lasting changes to the genes that cause diseases by precisely fixing, removing, adding, or disrupting specific sequences within those genes.
Casgevy works by taking bone marrow stem cells from a sickle cell patient, and changing the genetic material to reduce the problems caused by sickle cells. When these stem cells are replaced in the patient and used to make new red blood cells, the new red cells do not tend to sickle or cause other problems. The edited genes greatly increase the patient’s ability to make a fetal haemoglobin (HbF), which stops sickle haemoglobin damaging the red cells and reduces nearly all the symptoms caused by sickle haemoglobin.