In this concluding part, ARCHANA JYOTI learns from the team at AIIMS Delhi’s Surgical disciplines Department led by Dr. SUNIL CHUMBER, that while most thyroid nodules are benign and do not require immediate intervention, thorough evaluation is crucial to rule out malignancy. Close collaboration among patients, endocrinologists, radiologists, and surgeons is essential in managing thyroid nodules.
Does STN cause Cancer?
By Dr Catherine Halam & Dr Ankita Singh
The risk of cancer in a solitary thyroid nodule can vary depending on several factors, including the patient's age, gender, family history, and the characteristics of the nodule itself. Generally, the risk of cancer in a solitary thyroid nodule is estimated to be around 5-15%. However, it's important to note that the majority of thyroid nodules are benign (non-cancerous).
Several features of a thyroid nodule may increase the suspicion of cancer, including:
Size: Larger nodules tend to have a higher risk of cancer, although small nodules can also be malignant.
Age: Younger patients with thyroid nodules may have a higher risk of cancer.
Gender: Women tend to have a higher prevalence of thyroid nodules and thyroid cancer compared to men. However men with STN have a higher risk of malignancy.
Family history: A family history of thyroid cancer or certain genetic syndromes can increase the risk.
Radiological characteristics: Certain features seen on ultrasound, such as microcalcifications, irregular margins, increased vascularity, and taller-than-wide shape, may suggest a higher risk of malignancy.
Further there can be ‘Isolated thyroid nodule’ which is single swelling in the thyroid gland and the rest of the thyroid gland is normal or a ‘dominant thyroid nodule’ which is a single nodule that is felt prominently, while rest of the gland is also involved. It can be solid or cystic and have different risk of cancer based on gender: Isolate solid nodule in males- 48% (highest risk), Isolate solid nodule in females- 12%, Isolate cystic nodule in males- 24%, Isolate cystic nodule in females- 6%, Dominant solid nodule in male- 24%, Dominant solid nodule in females- 6%, Dominant cystic nodule in males- 12% and Dominant cystic nodule female- 4% (lowest risk).
Ultimately, the risk of cancer in a solitary thyroid nodule should be assessed on an individual basis, taking into account various clinical and diagnostic factors. If there is concern about cancer, further evaluation and management, including biopsy and possibly surgery, may be recommended by a healthcare provider.
Indications of Operation
By Dr. Piyush Ranjan & Dr. Amol Sood
Surgery may be indicated in a benign (non-cancerous) thyroid nodule if it is causing problems like difficulty in breathing or difficulty in swallowing. Surgical removal of the nodule may also be preferred by some patients if it is cosmetically disfiguring.
Nodules that are suspicious for cancer or cancerous should be removed surgically. Depending on the features of the nodule, the surgeon decides whether to proceed with the removal of only half of the thyroid gland containing the nodule or to remove the complete thyroid gland and also whether removal of the lymph nodes in the neck is required or not.
Nodules for which there is uncertainty whether they are benign or cancerous need further evaluation, in the form of either a repeat FNAB test a few weeks after the initial FNAB test, or molecular testing. A repeat FNAB test can be helpful as it may upgrade or downgrade the diagnosis of the nodule to either benign or cancerous, which can then be accordingly managed. If, however, the repeat FNAB test also classifies the nodule is indeterminate, surgery is the next step. Typically, in this surgery, the surgeon removes half of the thyroid gland containing the suspicious nodule and sends the removed part for examination under a microscope by a pathologist. No further treatment is required if the microscopic examination reveals no cancer. However, further surgery to remove the other half of the thyroid gland may be needed if cancer is seen on microscopic examination of the removed half of the thyroid gland.
Molecular testing looks at the genetic pattern of the thyroid nodule and classifies it as low-risk or high-risk for cancer. The use of molecular testing can help avoid surgery in low-risk indeterminate thyroid nodules, which can be kept under observation by routine ultrasound scans. However, the cost of these molecular tests can be prohibitive to many patients, who may then opt for surgical treatment.
Operations
By Dr. Rijuta Aphale & Dr. Piyush Ranjan
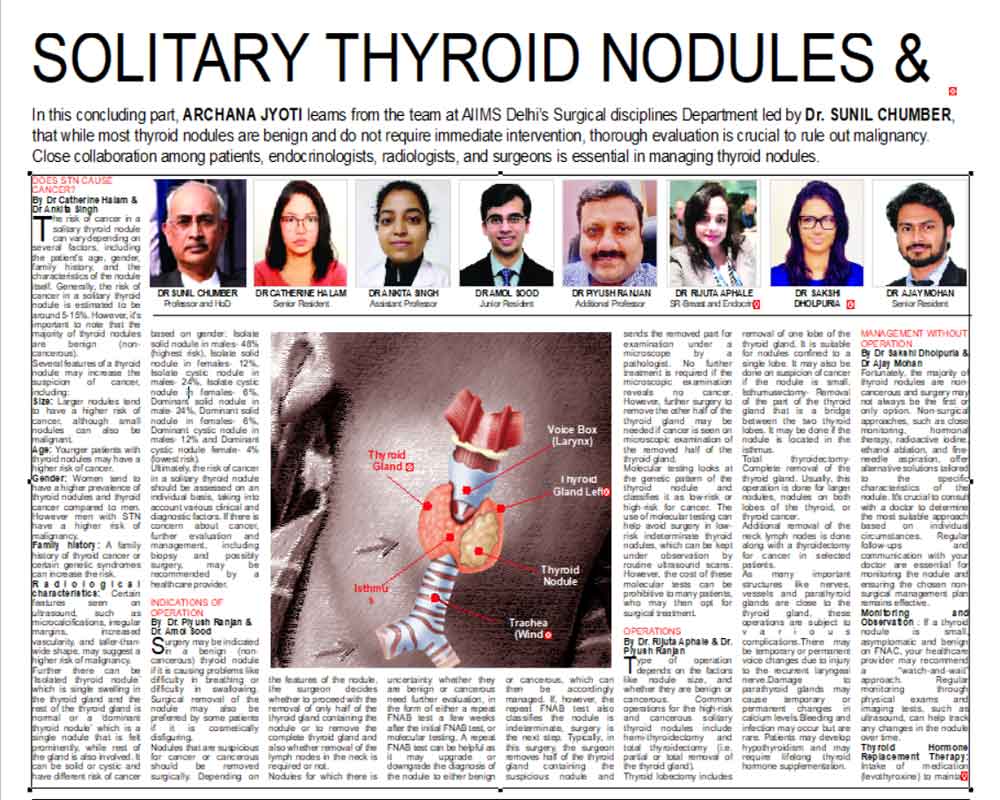
Type of operation depends on the factors like nodule size, and whether they are benign or cancerous. Common operations for the high-risk and cancerous solitary thyroid nodules include hemi-thyroidectomy and total thyroidectomy (i.e. partial or total removal of the thyroid gland).
Thyroid lobectomy includes removal of one lobe of the thyroid gland. It is suitable for nodules confined to a single lobe. It may also be done on suspicion of cancer if the nodule is small. Isthumusectomy- Removal of the part of the thyroid gland that is a bridge between the two thyroid lobes. It may be done if the nodule is located in the isthmus.
Total thyroidectomy- Complete removal of the thyroid gland. Usually, this operation is done for larger nodules, nodules on both lobes of the thyroid, or thyroid cancer.
Additional removal of the neck lymph nodes is done along with a thyroidectomy for cancer in selected patients.
As many important structures like nerves, vessels and parathyroid glands are close to the thyroid gland, these operations are subject to various complications.There may be temporary or permanent voice changes due to injury to the recurrent laryngeal nerve.Damage to parathyroid glands may cause temporary or permanent changes in calcium levels.Bleeding and infection may occur but are rare. Patients may develop hypothyroidism and may require lifelong thyroid hormone supplementation.
Management without operation
By Dr Sakshi Dholpuria & Dr Ajay Mohan
Fortunately, the majority of thyroid nodules are non-cancerous and surgery may not always be the first or only option. Non-surgical approaches, such as close monitoring, hormonal therapy, radioactive iodine, ethanol ablation, and fine-needle aspiration, offer alternative solutions tailored to the specific characteristics of the nodule. It's crucial to consult with a doctor to determine the most suitable approach based on individual circumstances. Regular follow-ups and communication with your doctor are essential for monitoring the nodule and ensuring the chosen non-surgical management plan remains effective.
Monitoring and Observation : If a thyroid nodule is small, asymptomatic and benign on FNAC, your healthcare provider may recommend a “watch-and-wait” approach. Regular monitoring through physical exams and imaging tests, such as ultrasound, can help track any changes in the nodule over time.
Thyroid Hormone Replacement Therapy: Intake of medication (levothyroxine) to maintain normal hormone level is required when the STN is associated with hypothyroidism. This may help shrink certain types of nodules.
Radioactive Iodine Therapy: This treatment involves taking a radioactive form of iodine, which is absorbed by the thyroid cells, reducing the size of the nodule in case of overactive nodules that produce excessive thyroid hormones.
Ethanol Ablation is a minimally invasive procedure that involves injecting ethanol (alcohol) directly into the thyroid nodule using ultrasound guidance. This treatment is often considered for cystic nodules, causing the fluid-filled portion to shrink.
Aspiration (Fine-Needle Aspiration) is more of a diagnostic procedure, but in some cases, it can also help drain cystic nodules with the help of a thin needle.